1. Describe some factors elicited in patient history that are relevant to airway management
- Surgical History: Especially interested in procedures that may affect cardiopulmonary physiology (e.g cardiac procedures, pneumenectomy) or spine mobility (e.g. cervical fusion).
History of problems with anesthesia: e.g. Post operative nausea and vomiting, Difficult placement of breathing tube, Delayed emergence, Awareness, Malignant Hyperthermia**
Drug Allergies and type of reaction: Specifically note egg allergies (Propofol exists in an egg-white emulsion). Allergies to chemicals that the body produces endogenously (e.g. epinephrine) should be taken with a grain of salt.
Current Medications and Doses: Confirm information if available in patient's chart.
Last meal: Consult NPO guidelines but, in general, patients should not have anything to eat in the last 8 hours.
Smoking history: _ packs/day for _ years. Smokers will have greater secretions (can be reduced with glycopyprolate) and may be more difficult to ventilate.
Do you have any problems with your lungs? e.g. Asthma, COPD, Snoring, TB
- If Asthma, ask how often albuterol is needed. Also ask about possible hospitalizations and intubations. If asthma history is alarming, nebulized albuterol will be provided prior to surgery.
- If snoring, ask if patient has received a sleep study (official diagnosis), and whether they use a CPAP at home.
2. What is the mallampati classification?
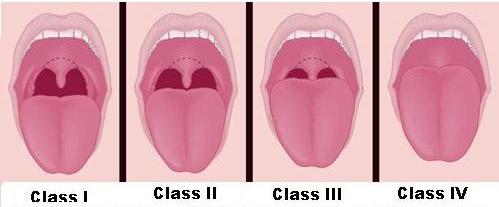
- Mallampati score: A measure of how large the tongue is in relation to the oropharynx. Ask patient to open their mouth wide and stick out their tongue as far as it will go (Do not ask them to say "aah"). Grade the airway based on the illustration below. Grade 3 or 4 is associated with difficult laryngoscopy.
3. Can you predict difficult mask ventilation? How would you deal with this problem?
An anesthetic history and physical exam can help predict if a patient will be difficult to mask ventilate:
- A history of previous difficult mask ventilation.
- Overweight patient with a lot of tissue around the face/neck.
- Facial hair.
- No teeth.
- OSA
- Large Tongue (Mallampati III or IV)
- Male
- Age > 55
- Airway masses.
Management of patient with difficult ventilation:
Pre-op
- Consider an alternative to general anesthesia.
- Consider an awake intubation if general anesthesia is necessary.
- Have a fiberoptic ready to go in case the patient is intubated and can't ventilate.
- Make sure to pre oxygenate the patient.
Intra-op
- Use an Oral Airway or LMA, and try to ventilate again.
- If you lose the ability to ventilate, and the airway can't be secured, emergency airways will be required (fiberoptic intubation, cricothyroidectomy, tracheostomy).
4. What are the indications for endotracheal intubation?
- The need to deliver positive pressure ventilation (e.g. under general anesthesia).
- Protection of respiratory tract from aspiration of gastric contents.
- Ensuring the airway remains patent
- Pulmonary toileting (e.g. removing mucus and secretions that may be causing atelectasis).
- Positioning (e.g. patient in prone position is more difficult to mask ventilate).
5. How do you confirm tracheal placement of ETT?
Four ways:
- Bilateral Chest Rise
- Condensation in the ETT
- ETCO2 on monitor (late finding)
- Resistance to airflow felt on ventilation bag.
6. What are complications of laryngoscopy and endotracheal intubation?
-
Traumatic Complications
- Airway Edema: Give dexamethasone after intubation to reduce swelling.
- Corneal Abrasion (by instruments): Cover eye with eye-tape.
- Bleeding: Suction blood to prevent aspiration.
-
Atraumatic Complications
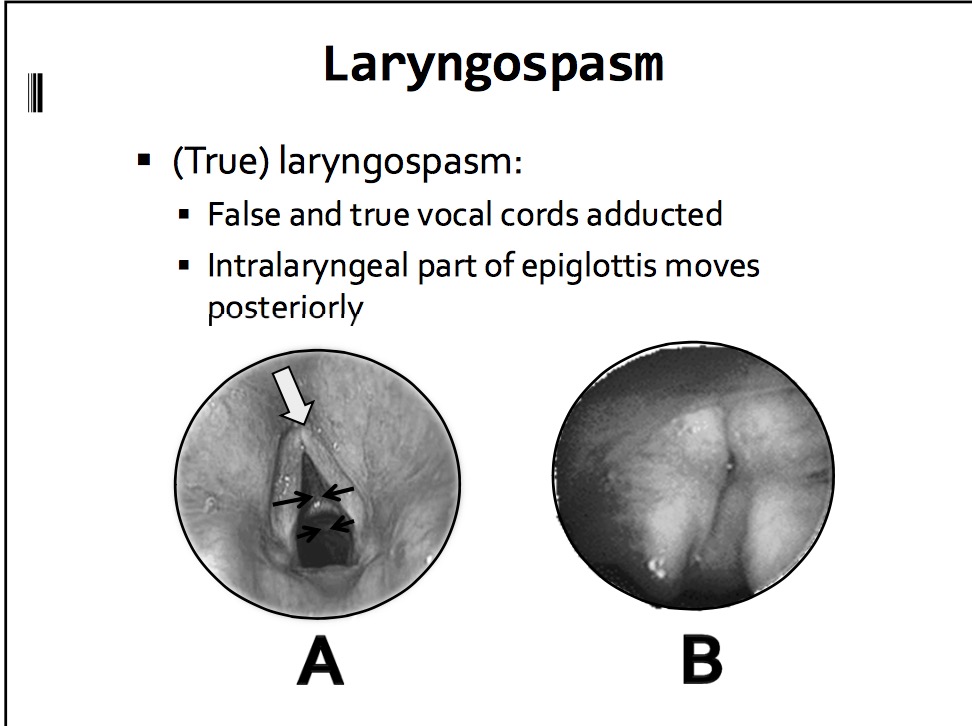
- Laryngospasm (i.e. mechanical airway irritation -> closure of true vocal cords (protective mechanism against aspiration) - > hypoxia): Deepen anesthesia and try to break with positive pressure ventilation. If unsuccessful, give succinylcholine to relax the vocal cords. If that fails, prepare for a surgical airway.
- Esophageal Intubation: Remove the tube without insufflating and try again. Suction air with orogastric tube before emergence.
- Catecholamine release in response to intubation: Give fentanyl before intubation to blunt airway responses. Ensure anesthesia is at sufficient depth before intubating.
- Right Mainstem Bronchus: Make sure you see bilateral chest rise and hear bilateral breath sounds after intubating.
7. What are some alternatives to laryngoscopy and oral intubation?
8. Describe some instances where use of an LMA would be contraindicated.
Absolute contraindications:
- High Aspiration Risk (LMA does little to protect the airway)
- Pathology of larynx that precludes mask placement.
Relative contraindications:
- PPV with airway pressure >20 mmHg (opening pressure of LES).
- Very long cases.
- Prone position.
For more information see here
9. What are the airway differences between children and adults?
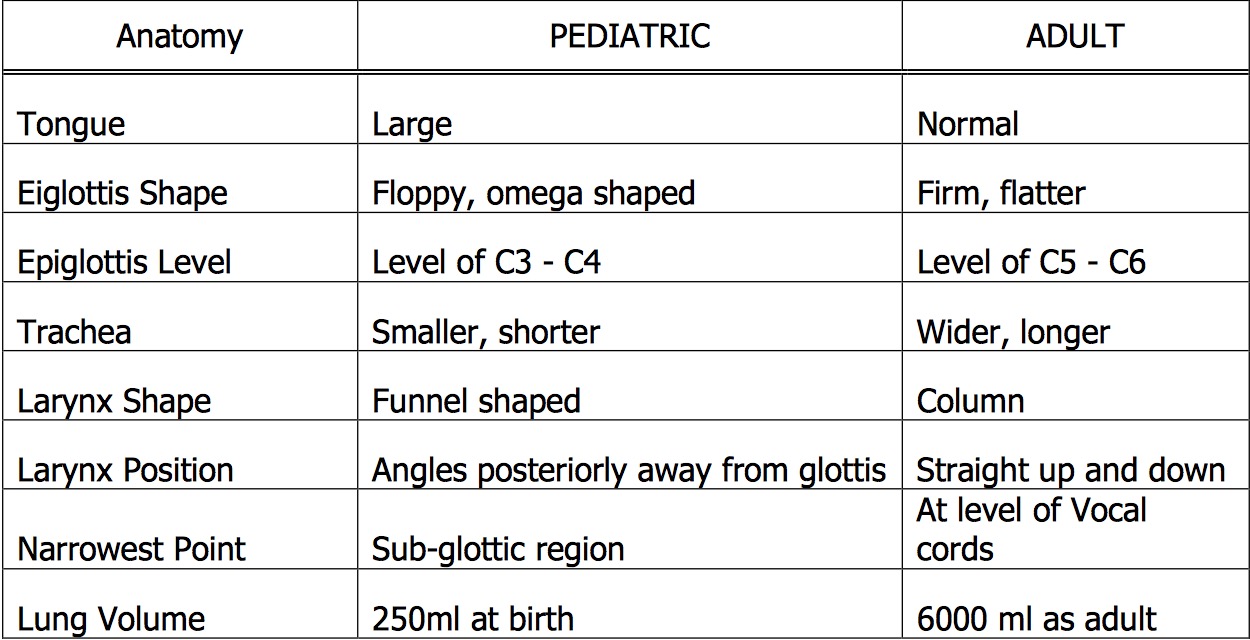
The respiratory mechanism of the pediatric patient varies from the adult in both anatomy and physiology. As children grow, the airway enlarges and moves more caudally as the c-spine elongates. The pediatric airway overall has poorly developed cartilaginous integrity allowing for more laxity throughout the airway. Another important distinction is the narrowest point in the airway in adults is at the cords versus below the cords for children. Some of the important anatomic differences are listed below.

An important aspect of the narrow airway in children is that resistance is significantly increased. The formula to consider is
R ~ 8l / r4
R – resistance, l – length, r – radius
Small changes in the airway radius will therefore increase the resistance to the fourth power. Therefore, a small amount of post-extubation sub-glottic edema will significantly increase the work of breathing for an infant. Children also have a smaller forced residual capacity (FRC) defined as the residual volume plus the expiratory reserve volume. Physiologically, FRC occurs when the outward pull of the chest wall equals the inward collapse of the lungs.
FRC essentially acts as a respiratory reserve. When patients begin to develop respiratory distress, an increased FRC equates to a longer period of time prior to respiratory failure. The reduced FRC is important in two particular circumstances. First, it can be decreased by up to 30% in a supine patient as compared to a sitting patient. As the abdominal contents push up on the diaphragm in a supine patient, the FRC is affected. This situation is amplified in pediatric patients because of a compliant chest wall, small thoracic cage, and large abdominal contents. Second, while pre-oxygenating a patient prior to intubation the reduced FRC decreases the amount of time allowed to establish an endotracheal tube prior to desaturation.
There are also many physiologic differences in respiratory mechanisms between children and adults. Children have a more complaint trachea, larynx, and bronchi due to poor cartilaginous integrity. This in turn allows for dynamic airway compression, i.e. a greater negative inspiratory force “sucks in” the floppy airway and decreases airway diameter. This in turn increases the work of breathing by increasing the negative inspiratory pressure generated. A vicious cycle is created which may eventually lead to respiratory failure: subglottic stenosis ⇒ ⇑ negative inspiratory force ⇒ airway collapse ⇒ ⇑ subglottic stenosis ⇒ ⇑ negative inspiratory force ⇒ ⇑ work of breathing ⇒⇒ respiratory failure. Pediatric patients also have more compliant chest walls also increasing the work of breathing – i.e. the outward pull of the chest is greater.
Infants are dependent on functional diaphragms for adequate ventilation. The accessory muscles contribute less to the overall work of breathing in infants as compared to older children and adults. Therefore, a non-functional diaphragm often leads to respiratory failure. Diaphragmatic fatigue is one amongst several potential causes of respiratory failure and apnea in young patients with RSV bronchilitis.
Finally, the respiratory muscles themselves have a significant oxygen and metabolite requirement in children. In pediatric patients the work of breathing can account for up to 40% of the cardiac output, particularly in stressed conditions.
This cursory discussion of the pediatric respiratory anatomy and physiology allows one to appreciate the significant differences between children and adults. Therefore, the child with respiratory distress / failure should be approached and treated with urgency, vigilance, and caution.
10. What is laryngospasm and how is it treated?
- Mechanism: mechanical airway irritation -> closure of true vocal cords (protective mechanism against aspiration) - > hypoxemia +/- hypercapnia +/- increased respiratory effort +/- inspiratory stridor
-
Prevention:
- Ensure adequate anesthetic depth before manipulating patient.
- Clear secretions before extubation.
- Topicalize larynx with local anesthetic
- Muscle relaxants
- Consider antisialogue
-
Management: (AFTER calling for help)
- Jaw thrust, head tilt, oral airway
- Deepen anesthetia with IV agent
- CPAP via bag mask with 100% O2
- Suction oropharynx
- Sux 10-20 mg IV
- Prepare for surgical airway
- Monitor for post-obstructive negative pressure pulmonary edema.
11. What is bronchospasm and how is it treated?
Definition: Constriction of small intrathoracic airway causing obstruction of expiratory air flow.
Signs:
- Bilateral expiratory wheezing
- Prolonged expiratory phase
- Increased peak airway pressures.
Mechanism:
- Allergic reaction (hypotension will occur early in the process)
OR
- Susceptible airway (history of smoking, asthma, respiratory tract infection)
- +/- Airway irritation with inadequate anesthesia depth.
- +/- Pharmacologic-induced histamine release
Differential: Endobronchial intubation, pneumothorax, pulmonary edema, esophageal intubation.
Cardiopulmonary effects: V/Q Mismatch, RV overload/failure, Decreased venous return and hypotension.
Intra-op Management:
- 100% O2
- Deepen anesthesia
- Manual ventilation to assess compliance
- Provide adequate expiratory time.
- Avoid PEEP.
- Albuterol
- Epinephrine ONLY for anaphylactic bronchospasm
- If still persists, MgSO4 40mg/kg IV over 20 min
- Consider steroids.
12. Why are patients pre-oxygenated?
Normally lung reserve volume only contains 21% oxygen. By delivering patients 100% oxygen (and asking them to breathe deeply), air in the lungs (specifically the FRC) is replaced by 100% oxygen. This is done until the Expiratory O2 is >80-90%. Normally the body requires 250 cc of oxygen per minute. The FRC is 2500 cc. Therefore, by preoxygenating, the body has enough oxygen in the lungs to allow patients to be apneic for upto 10 minutes.
13. Describe the difficult airway algorithm.
See here