1. Why are patients questioned about sleep apnea
Patients with sleep apnea are at greater risk for being more difficult to ventilate (because anesthetic agents cause airway muscle relaxation), for becoming hypoxemic intraopeeratively, and being more difficult to extubate.
2. What are some of the common risks and side effects of anesthesia to discuss pre-op?
Some of the more common risks of anesthesia that need to be mentioned include infection and bleeding if a regional block is to be placed, nerve injury from positioning or regional blocks, postoperative nausea and vomiting, dental damage, risk of viral hepatitis and HIV from blood transfusions, awareness under anesthesia and a need for postoperative mechanical ventilation (patient fails extubation after surgery ends).
3. What are the specific areas targeted in the pre-op physical exam?
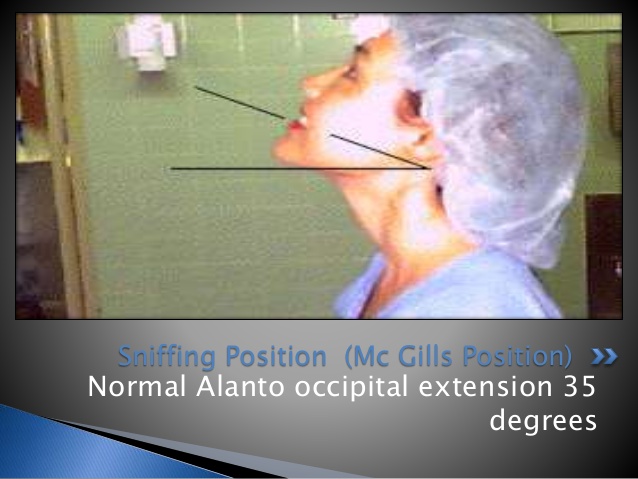
- Neck Range of Motion: Ask patient to assume sniffing position (cervical flexion and atlanto-occipital extension), the position they will be in while being intubated. Normal patients should achieve 35 degrees or more of extension without pain, tingling or numbness.
- TMJ mobility and degree of mouth opening: Required to determine adequacy of space for manipulating laryngoscope.
- Measure Inter-incisor distance (<2 finger breadths = difficult intubation predicted).

Upper lip bite test: Ask patient to move lower incisors as high on the upper lip as possible (if lower teeth do not reach vermilion of upper lip, sign of inadequate TMJ movement).
Dentition: Note the presence of dentures, poor dentition, loose teeth or caps, which may not tolerate digital manipulation or be at risk of damage when the laryngoscope blade is inserted. Patients with large incisors are difficult to intubate. Edentulous patients are easier to intubate but difficult to ventilate.
Tongue/Oropharynx: * Direct laryngoscopy allows visualization of the larynx by displacing the tongue anteriorly into the mandibular space, which moves the tongue out of the line of sight. A normal sized tongue will generally fit easily into the space between the two mandibular rami. However, if the tongue is too large (macroglossia) or the mandible is too small (micrognathia), there will likely be difficulty with proper visualization of the glottis.
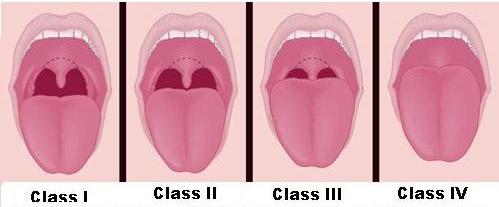
Mallampati score: A measure of how large the tongue is in relation to the oropharynx. Ask patient to open their mouth wide and stick out their tongue as far as it will go (Do not ask them to say "aah"). Grade the airway based on the illustration below. Grade 3 or 4 is associated with difficult laryngoscopy.
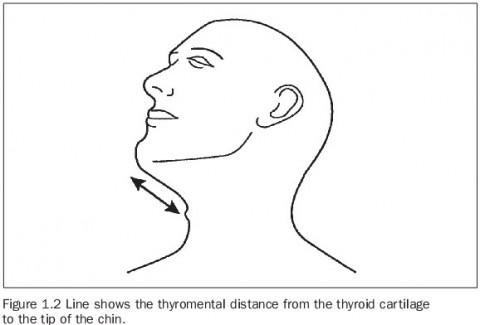
- Thyromental Distance: Assesses the size of the mandible. Distance from the mandible mentum to the thyroid cartilate. Difficult intubation if thyromental distance < 3 finger breadths.
4. Discuss the ASA physical status classification
All conditions that may have an impact on the anesthetic management are addressed and specific recommendations are made. Based on the history a physical status is assigned to the patient. The American Society of Anesthesiologists (ASA) Physical
Status Classification is as follows:
- ASA 1 Patient with no systemic disease
- ASA 2 Patient with mild systemic disease
- ASA 3 Patient with severe systemic disease that limits activity
- ASA 4 Patient with incapacitating disease that is a constant threat to life
- ASA 5 Patient that is moribund and not expected to survive 24 hours
In the event of emergency surgery the letter E is added to the classification
The ASA classification is not an assignment of anesthetic risk. It is one way that anesthesiologists use a common language to describe patients to each other.
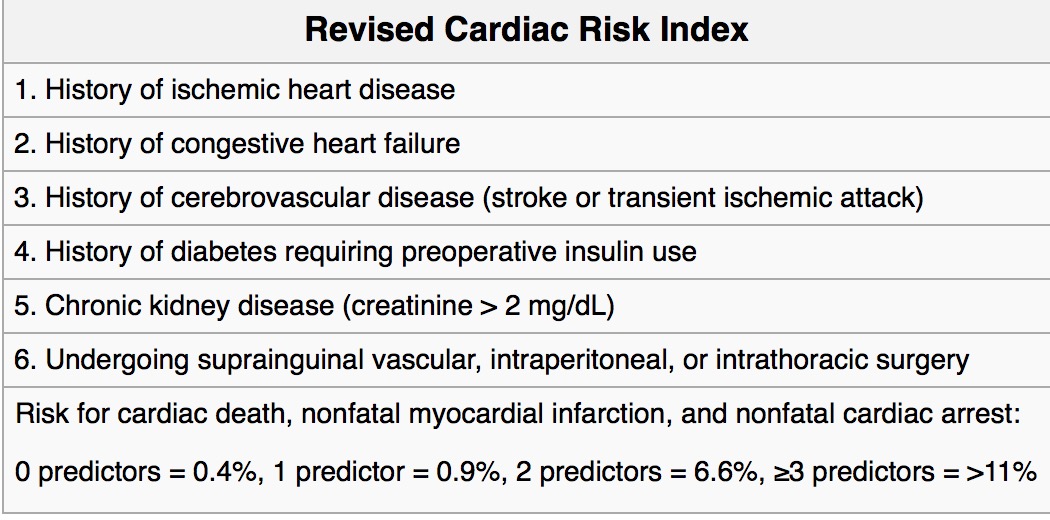
5. What are the clinical predictors of cardiac risk?
6. Discuss the risk factors for post-op pulmonary complications.
Risk factors:
- Age
- Obesity (body mass index of >27 kg/m2) causes a reduction in lung volume, ventilation-perfusion mismatch, and relative hypoxemia, which are accentuated after surgery)
- Poor exercise capacity
- Weight loss (albumin < 3.5)
- Smoking: 2x risk even in the absence of COPD. The risk is highest in patients who smoked within the last 2 months. Patients who quit smoking for more than 6 months have a risk similar to those who do not smoke.
- COPD
- Asthma: increases the risk of bronchospasm, hypoxemia, hypercapnia, inadequate cough, atelectasis, and pulmonary infection following surgery.
- Pulmonary Hypertension: Increased risk of mortality, congestive heart failure, hemodynamic instability, sepsis, and respiratory failure, and they had longer ICU and hospital length of stay and increased readmission rates.
- Interstitial lung disease Sleep apnea Increased risk of developing deterioration of sleep-disordered breathing, severe hypoxemia, and hypercapnia in the postoperative period. The risk of aspiration pneumonia, acute respiratory distress syndrome, and pulmonary embolism are all greater among patients with obstructive sleep apnea. Intraoperative sedatives and opioids should be minimized
- Surgical Site: Closer to the diaphgram, greater the risk of post-op pulmonary complications.
- Surgical Duration: Longer the surgery, greater the risk.
- Absence of neuraxial pain control: Presece of spinal or epidural anesthesia (alone or with general anesthesia) REDUCES the risk of post-op pulmonary complications.
7. How does duration of smoking cessation affect post-op risk of pulmonary complications?
The risk of pulmonary complications is highest in patients who smoked within the last 2 months. Patients who quit smoking for more than 6 months have a risk similar to those who do not smoke.
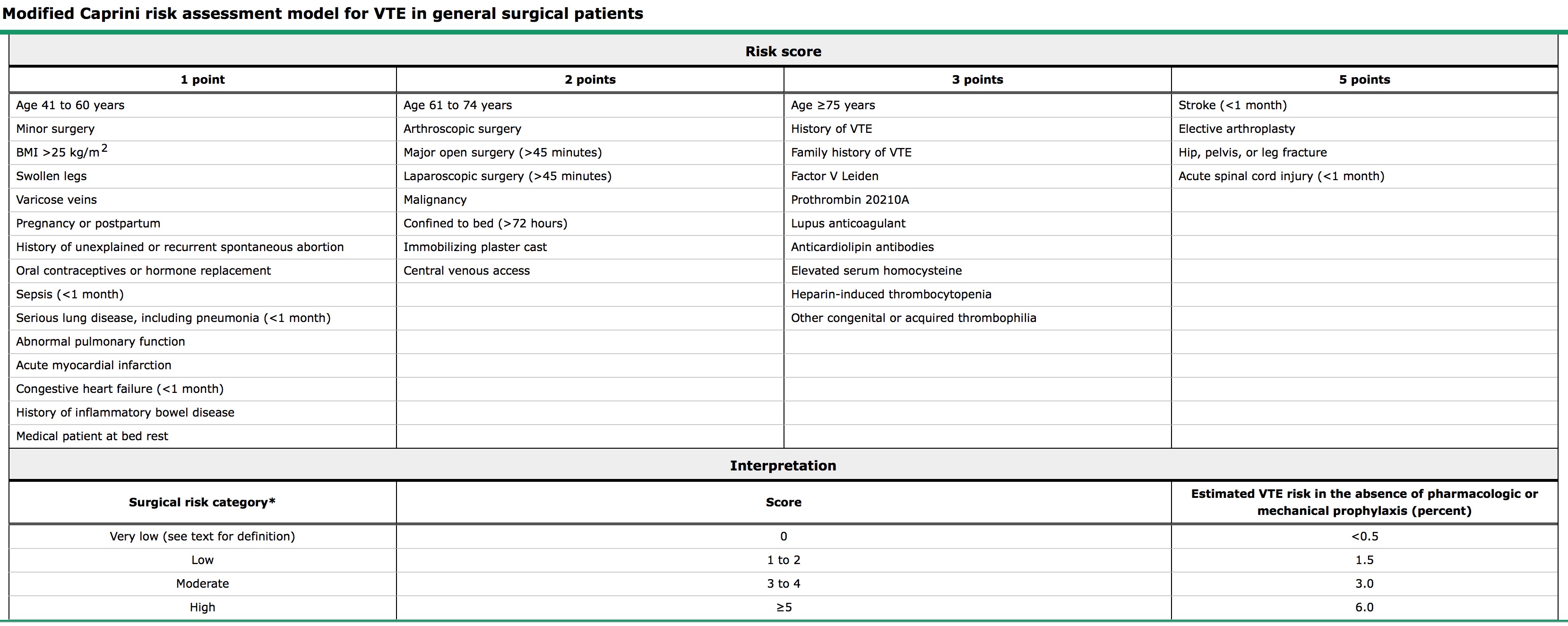
8. How is thromboembolic risk stratified? What measures are used to prevent DVTs?
Modified Caprini Criteria are used to stratify DVT risk. In general risk is increased by:
- Increasing Age
- Personal or Family history of DVTs
- Presence of malignancy or obesity
- Presence of hypercoagulable state
- One or more significant medical comorbidities.
Management:
- Very Low Risk: Early and frequent ambulation
- Low Risk: Sequential compression devices
- Moderate/High Risk: Pharmacologic prophylaxis (LWM Heparin is preferred)
- High Risk: Sequential compression devices AND pharmacologic prophylaxis
Complete Caprini Criteria
9. What are some patient risk factors for pulmonary aspiration?
- Full stomach/unknown NPO status
- Intra-abdominal process (bowel obstruction, ileus, inflammation)
- Gastroparesis (narcotics, DM, uremia, EtOH, infection)
- GE junction incompetence (GERD, hiatal hernia, scleroderma
- Pregnancy
- Obesity
- Neuromuscular diseases
- Difficult intubation/prolonged bag-mask ventilation.
10. Discuss the medications which could be helpful reducing the risk of pulmonary aspiration.
Medications given to at-risk patients:
- Metoclopramide
- H2 blockers
- antacids
- Proton Pump Inhibitors
NB: There is no evidence that these medications actually reduce risk of pulmonary aspiration.
11. Review the NPO guidelines for elective surgery.
| Liquid and Food Intake | Minimum Fasting Period |
|---|---|
| Clear Liquids | 2 |
| <3 year old | 6 |
| >3 year old | 8 |