1. Classify Neuromuscular blockers.
Non-depolarizing neuromuscular blockers (exert their effect through competitive antagonism ofnicotinic acetylcholine receptors): All blockers ending in _-ium.
Depolarizing neuromuscular blockers (exert their effect through activation and persistent depolarization of post-synaptic acetylcholine receptors): Succinylcholine
2. What is the choice of NBMD influenced by?
Choice of which neuromuscular blocker to use depends on several factors:
Whether rapid sequence intubation is required (will usually use succinylcholine for fast onset/offset or double dose rocuronium for fast onset).
Whether there are contraindications to succinylcholine (e.g hyperkalemia, prolonged immobility, burns).
Whether nerve monitoring will be required during the surgery. In cases requiring recurrent nerve monitoring neuromuscular blockers are not given.
For emergency paralysis (e.g. laryngospasm), succinylcholine is typically use because of its immediate onset (~30 sec).
In renal of hepatic cases, cisatracurium may be useful as it is degraded by plasma esterases and Hoffman elimination.
Certain diseases are resistant to non-depolarizing NMBA (e.g. Guillain-Barre, Burns, Spinal Cord Injury, CVA, prolonged immobility).
Specific Drug Selection Guidelines (UNC):
-
Pancuronium
- when duration of relaxation needed is longer than 1 hour
- when extubation is not planned immediately post-op
- when renal function is normal
- when patient < 70 years old
- when no comorbidity factors are present. This incorporates the data that suggests the immediate-acting (duration drugs) are more easy to reverse than pancuronium.
-
Cisatracurium
- presence of renal failure
70 years old
- when complete reversal of NMB is absolutely essential at end of case (e.g. full stomach, morbid obesity, difficult airway, etc.) duration of case 35-60 minutes
-
Vecuronium
- when complete reversal of NMB is absolutely essential at end of case (e.g. full stomach, morbid obesity, difficult airway, etc.) duration of case 35-60 minutes
-
Mivacurium
- profound relaxation needed in case no longer than 35 minutes a succinylcholine drip, made by combining 5 (20mg/cc x 10cc) bottles is another valid alternative to mivacurium
-
Rocuronium
- when succinylcholine is contraindicated
- when complete reversal of NMB is absolutely essential at end of case (e.g. full stomach, morbid obesity, difficult airway, etc.)
-
d-tubocurarine
- can be used to prevent fasciculations induced by succinylcholine when administered 3 to 5 minutes prior to the dose of succinylcholine
The following drugs have not been deemed to have clinical value our operating room:
- doxacurium
- gallamine
- metocurine
- pipecuronium
3. What is the intubating dose of succinylcholine?
- 1 to 1.5 mg/kg.
- If using a defasciculating dose of rocuronium (0.03 mg/kg), intubating dose is higher (1.5-2 mg/kg).
4. How is succinylcholine metabolized?
Rapidly metabolized by pseudocholinesterases (Duration ~ 10 min) (as opposed to hepatic metabolism, which takes longer).
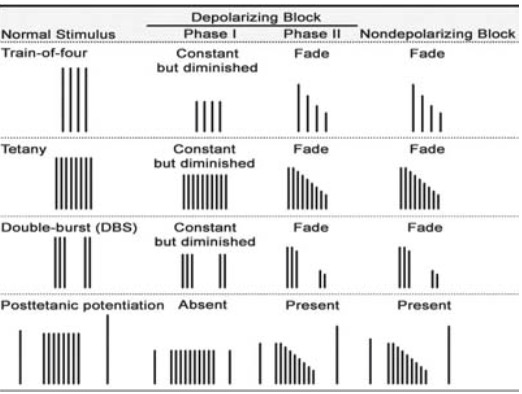
5. Describe the difference between Phase 1 and Phase 2 block
Phase 1 is the depolarizing phase where muscle fibers are depolarized and fasiculations occur.
Phase 2 is the desensitizing phase in which the muscle is no longer responsive to acetylcholine released by motor neurons. At this point, full neuromuscular block has been achieved.
6. What is the Dibucaine number? Describe its use.
- A dibucaine test is used to test for abnormal plasma cholinesterase. The dibucaine number is the percent of pseudocholinesterase enzyme activity that is inhibited by dibucaine.
7. What are the side effects of succinylcholine? How can these be reduced?
Side Effects:
- Hyperkalemia: Causes an increase in K of 0.5 mEq/L.
- Giving sux to patients at risk for upregulation of nAChR on muscle cells (e.g. prolonged immobility, stroke, muscular dystrophy, burn injury) may result in hyperkalemic arrest.
- Malignant Hyperthermia
- Bradycardia (especially in children). Often given with atropine.
- Tachycardia (due to catecholamine release).
- Anaphylaxis (approx. 1:5000 - 1:10,000)
- Fasciculation + Myalgia.
- Trismus
- Increased intracranial pressure, intraocular pressure and intragastric pressure.
Prevention of side effects:
Myalgias and increased ICP might be prevented with a defasciulating dose of rocuronium (0.03 mg/kg 3 minutes prior to sux). This will NOT prevent hyperkalemia or increased intraocular pressure.
8. Which NMBD’s have an effect on the cardiovascular system. How are these effects exerted?
Succinylcholine: Risk of hyperkalemic arrhythmias/arrest, bradycardia (due to stimulation of muscarinic receptors in sino-atrial node). Eliminated by pseudocholinesterase.
For the other neuromuscular blockers, cardiovascular effects (if present) are normally due to histamine release. Specific effects and elimination patterns are below;
| Drug | Potency* | ED95
(mg/kg) |
Duration
ED95 (min) |
Cardiovascular Effects | Elimination |
| Pancuronium | 1 | 0.07 | ~60 | ↑HR, ↓BP | 60% kidney 40% liver |
| Gallamine | 0.025 | 2.8 | ~60 | ↑HR, ↓BP | 100% kidney |
| Curare | 0.14 | 0.5 | ~60 | Histamine release ¯↓BP,
ganglionic blockade |
40% kidney 60% liver |
| Metocurine | 0.25 | 0.28 | ~60 | 1/3 histamine of curare ¯↓BP,
ganglionic block |
60-90% kidney |
| Vecuronium | 0.9 | 0.056 | ~25 | None | 50% liver 20% kidney |
| Atracurium | 0.25 | 0.26 | ~25-30 | 1/3 histamine of curare ¯↓BP | Nonspecific plasma esterases,
Hoffmann elimination |
| Mivacurium | 0.875 | 0.08 | ~19 | similar to atracurium | Hydrolysis: plasma cholinesterase |
| Doxacurium | 2.3 | 0.03 | ~60 | minimal ¯↓BP | ~50% kidney |
| Pipecuronium | 1.4 | 0.05 | ~60 | None | 75% kidney |
| Rocuronium | 0.23 | 0.3 | ~25-30 | None, ? ↑HR | ~ 50% liver ~ 20% kidney |
| Cisatracurium | 1.4 | 0.05 | ~25-30 | None | Hoffmann elimination |
9. Which NMBD's are eliminated primarily through the kidneys, and which through the liver?
| Drug | Potency* | ED95
(mg/kg) |
Duration
ED95 (min) |
Cardiovascular Effects | Elimination |
| Pancuronium | 1 | 0.07 | ~60 | ↑HR, ↓BP | 60% kidney 40% liver |
| Gallamine | 0.025 | 2.8 | ~60 | ↑HR, ↓BP | 100% kidney |
| Curare | 0.14 | 0.5 | ~60 | Histamine release ¯↓BP,
ganglionic blockade |
40% kidney 60% liver |
| Metocurine | 0.25 | 0.28 | ~60 | 1/3 histamine of curare ¯↓BP,
ganglionic block |
60-90% kidney |
| Vecuronium | 0.9 | 0.056 | ~25 | None | 50% liver 20% kidney |
| Atracurium | 0.25 | 0.26 | ~25-30 | 1/3 histamine of curare ¯↓BP | Nonspecific plasma esterases,
Hoffmann elimination |
| Mivacurium | 0.875 | 0.08 | ~19 | similar to atracurium | Hydrolysis: plasma cholinesterase |
| Doxacurium | 2.3 | 0.03 | ~60 | minimal ¯↓BP | ~50% kidney |
| Pipecuronium | 1.4 | 0.05 | ~60 | None | 75% kidney |
| Rocuronium | 0.23 | 0.3 | ~25-30 | None, ? ↑HR | ~ 50% liver ~ 20% kidney |
| Cisatracurium | 1.4 | 0.05 | ~25-30 | None | Hoffmann elimination |
10. How is neuromuscular blockade monitored?
- Train of four ratio is most commonly used to monitor depolarizing NMBDs.
- Twitch # and twitch height are assessed by feel/sight or using a muscle monitor.
Surgical relaxation can be achieved when a patient has 2-3 twitches.
Different muscle groups respond differently to blockade.
(Most resistant to most sensitive): Vocal cords > diaphragm > currogator supercilii (muscle controlling the eyebrow) > abdominal muscles > adductor pollicis > pharyngeal muscles > extraocular muscles.
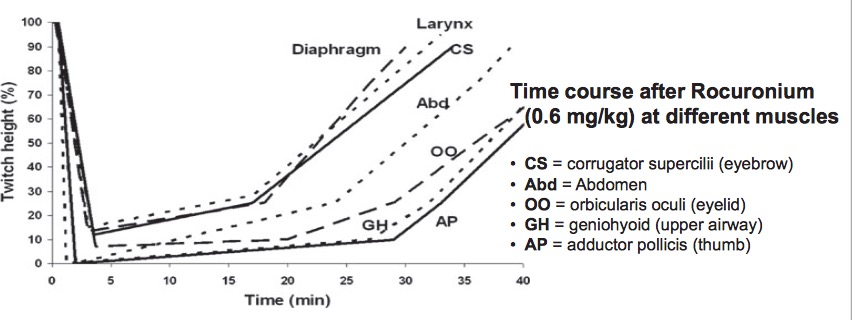
- Since pharyngeal muscles are one of the last muscles to recover, inadequate reversal can cause airway obstruction and aspiration.
11. How does train of four differ with depolarizing and non-depolarizing drugs? Phase 1 and Phase 2 Blocks?
12. How are NMBD's antagonized? Describe the typical combination of drugs used and the rationale for their use.
Anticholinesterase "reversal agents" indirectly increase the amount of Ach in the NMJ by inhibiting acetylcholinesterase.
Anticholinesterases cause vagal side effects (bradycardia, GI stimulation, bronchospasm) by increasing ACh activity at parasympathetic muscarinic receptors. Anticholinergics should always be co-administered.
Neostigmine (40-50 mcg/kg) with glycopyrolate (20% of neostigmine dose) most commonly used. Ceiling effect (Do not give >70 mcg/kg of neostigmine). Pyridostigmine and Edrophonium can also be used.
-
Pair anticholinesterase and anticholinergics based on speeds of onset.
- Edrophonium (rapid) w/ atropine
- Neostigmine (intermediate) w/ Glycopyrolate
- Pyridostigmine (slow) w/ glycopyrolate.
Unlike the above drugs, Physostigmine crosses the BBB and can be used to treat central anticholinergic syndrome/atropine toxicity.
13. Does reversal increase the risk of PONV?
- Reversal does not increase the risk of PONV.
14. How is the adequacy of recovery from NMBD's evaluated.
- Reversal should not be given until spontaneous recovery has started (e.g. until 4 twitches are visible) because reversal agents can paradoxically slow recovery if given too early.
15. What are cases where Neuromuscular blockers cannot be used? What are alternatives?
- Cases involving nerve monitoring (frequent in neuro and ENT cases). At sinai a remifentanil/Propofol infusion is run through the case to induce deep anesthesia and immobility.
In these cases, a laryngneal tracheal anesthetic (LTA, usually 4% Lidocaine) is administered directly on the vocal cords to relax the vocal cords and allow the endotracheal tube to enter.
16. What is the mechanism of action for succinylcholine?
Succinylcholine resembles two adjoined Acetylcholine molecules. It causes persistent depolarization of muscles by attaching to ACh receptors on the motor end plate.
17. What is the mechanism of action for rocuronium?
Competitive antagonism of post-synaptic acetylcholine receptors.
18. Why are neuromuscular blockers given?
- Surgical Immobility.
- Ease intubation (by relaxing pharyngeal muscles.
- To treat laryngospasm.