1. What are the physiological components of mean arterial pressure (MAP)?
- Two equations to know:
- Mean Arterial Pressure = 1/3 x (Systolic Blood Pressure) + 2/3 (Diastolic Blood Pressure)
- Mean Arterial Pressure = Cardiac Output x Systemic Vascular Resistance.
Blood pressure cuff measures MAP and uses an algorithm to determine SBP and DBP.
2. How is blood pressure measured in the OR? Discuss the pros and cons of the different techniques.
Non-Invasive Blood Pressure Monitoring (NIBP): This refers to a blood pressure cuff cycling blood pressures every 5 minutes during the surgery.
PROS: Non-Invasive.
Cons: Can be inaccurate (e.g. if cuff size is not appropriate), Cannot detect continuous("beat-to-beat") blood pressure.
Invasive Arterial Line: A transducer is connecting to the radial artery (chosen because of easy to access location and collateral blood supply from ulnar artery). The transducer is zeroed to atmospheric pressure, then measures the arterial pressure from the radial artery.
PROS: Provides continuous ("beat-to-beat") blood pressure rather than q5min, the measured blood pressure is very accurate. Also allows for frequent blood sampling and ABG analysis.
Cons: Infections, small possibility of a hemorrhage, may be difficult to obtain access in patients with poor arteries (e.g. renal patients).
Indications: Patients with a history of cardiac problems where intraoperative hypotension needs to be avoided, surgery where beat to beat monitoring is essential.
3. What is the differential diagnosis for tachycardia under general anesthesia?
- Stimulation due to light anesthesia/Pain: (check BIS, deepen anesthesia).
- Hypotension/Hypovolemia: (Check fluid status, consider Phenylephrine, which will raise blood pressure but not heart rate)
- Hypoxia/Hypercarbia
- Hyperthermia
- Medications: e.g. Desflurane
- Thyroid Storm
- Far less common: Malignant hyperthermia, Serotonin Syndrome, Neuroleptic Malignant Syndrome
4. How do both tachycardia and bradycardia cause a low cardiac output?
Cardiac Output = Heart Rate x Stroke Volume.
Bradycardia: By decreasing heart rate, you decrease the per minute ejection of blood from the heart.
Tachycardia: If the heart rate is too fast, there may be insufficient diastolic filling, leading to a decreased stroke volume. Most crucial in patients with Aortic Stenosis and Hypertrophic Obstructive Cardiomyopathy as they depend on atrial push to sustain stroke volumes.
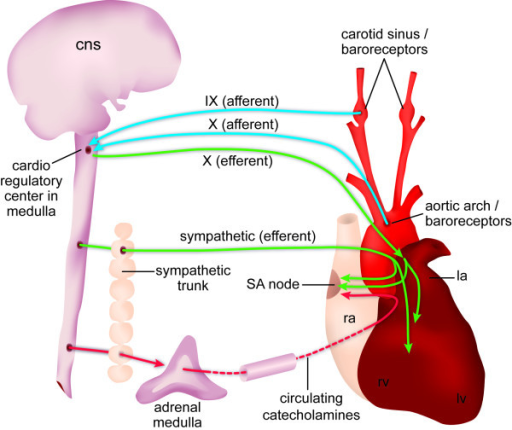
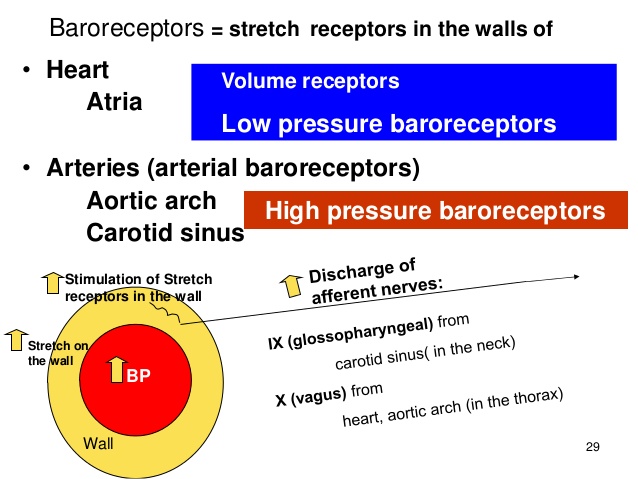
5. Discuss the functions of the carotid sinus baroreceptor.
- Stretch receptors in the Carotid Sinus wall sense blood pressure elevations and send signals via the CN IX to increase heart rate.
6. What effect does tachycardia have on left ventricle perfusion?
Tachycardia decreases left ventricular perfusion because it decreases diastolic filling time (the period when blood enters coronary circulation).
7. Describe hypoxic pulmonary vasoconstriction
In the lungs, hypoxia causes pulmonary arteries to vasoconstrict in order to divert blood flow towards alveoli with higher oxygen content. This minimizes V/Q mismatch. Commonly seen in COPD, high altitude, pulmonary embolism and CHF.
8. What are the west zones of the lung?
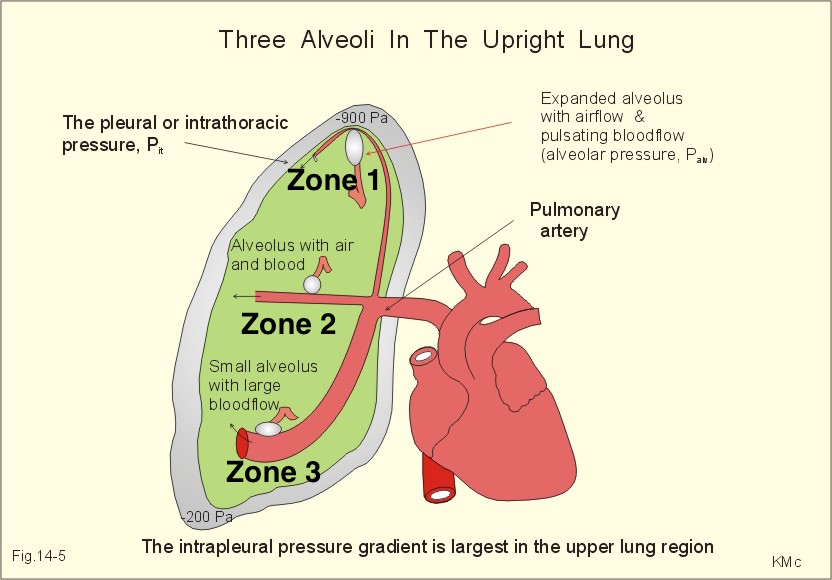
The West (named after a person) zones of the lung refer to three segments of the lung which have different ventilation and perfusion.
-
In an upright individual:
Zone 1 has the greatest ventilation (because air rises) but poorest perfusion (because gravity pulls blood downwards).
Zone 2 is middle ground (intermediate ventilation and intermediate perfusion).
Zone 3 has greatest perfusion (because blood is pulled down by gravity) and lowest ventilation.
ZONE 3 (not 2) has the least V/Q mismatch because the difference in perfusion between zones is large while the difference in ventilation is small.
9. What events shift the oxyhemoglobin dissociation curve to the right? What does a right shift mean in physiological terms?
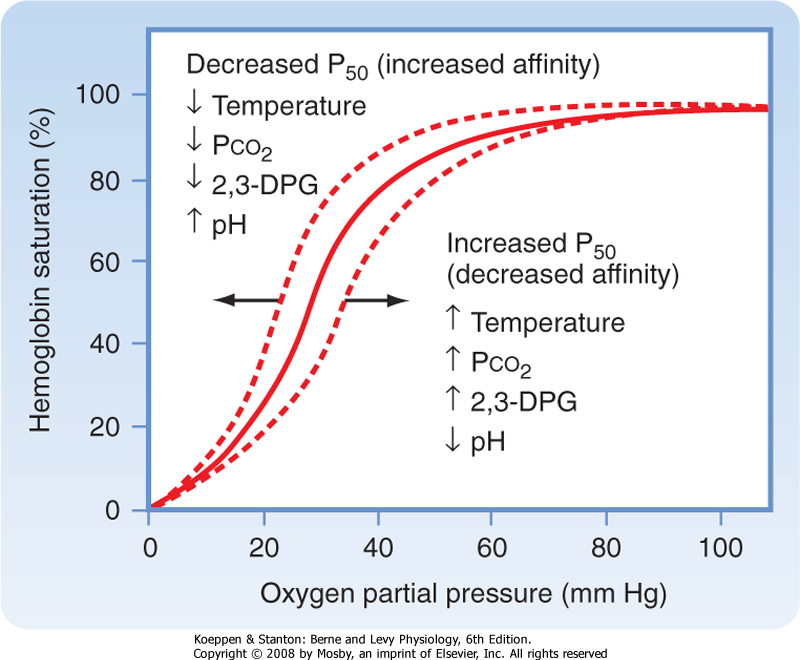
In physiological terms, a right shift means hemoglobin has decreased affinity for oxygen. This is usually seen in areas where oxygen needs to be delivered to (e.g. tissues and organs)
10. What is anatomic and alveolar dead space?
Dead Space = An area of good ventilation but poor perfusion.
Anatomic dead space: The part of the airway that conducts air from the mouth to the bronchioles.
Alveolar dead space: Sum of volumes of alveoli with no blood flowing through their surrounding capillaries. Normally low, but can rise quickly in patients with V/Q mismatches (e.g. pulmonary embolism). 
11. Describe the hypercapnic ventilatory response. How do opioids affect this response?
Central chemoreceptors in the brain increase ventilation in response to CSF acidity. Greater CO2 concentration in the blood makes the blood more acidic, and so increases the rate of ventilation (as a means to remove CO2 from the blood).
The central chemoreceptors can also detect changes in PaCO2. However, they are not sensitive to changes in PaO2. Therefore Hypoxia is not as strong a driver for ventilation and hypercapnia.
The peripheral chemoreceptors include the carotid bodies and the aortic bodies. The carotid bodies are much more important than the aortic bodies in humans. The peripheral chemoreceptors are sensitive to hypoxia and hypercapnia/acidosis.
Opioids blunt the ventilatory response, and so lead to resting hypercapnia.
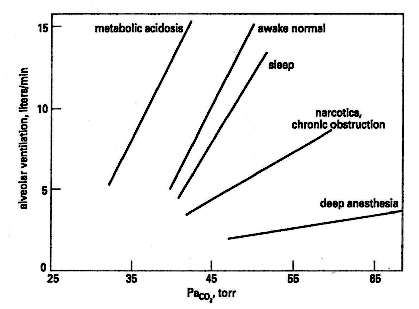
Figure: The effects of sleep, narcotics, chronic pulmonary obstructive pulmonary disease, deep anesthesia, and metabolic acidosis on the ventilatory response to carbon dioxide. From MG Levitzky, Pulmonary Physiology, 5th ed.
12. What is the most potent inotrope?
Calcium. This is why it is especially important to maintain the levels of calcium intraoperatively.