Pre-Oxygenation
Patients are routinely preoxygenated. By filling the functional residual capacity of the lungs with 100% oxygen, a longer period (~10 min) of apnea can be tolerated without arterial desaturation occurring.
Gently hold the face mask over the patient's airway, make a seal (your attending will show you how) and ask the patient to take deep breaths (to ensure that all the air in the lungs is displaced by oxygen). If there is a good seal, you should see a waveform on the capnography monitor and a normal End Tidal CO2 of 35-45.
The attending will administer induction agents. Propofol burns, so the patient may try to speak. Reassure the patient that this is normal, but DO NOT remove the mask. Once the mask is removed and room air enters the lungs, the entire preoxygenation process needs to be restarted from scratch.
Preoxygenate until the End Tidal O2 is ~90% (you can check this on the monitor display).
As the induction agents start acting, you patient will become apneic.
Once the patient is apneic, you will mask ventilate (you attending will show you how).
Mask Ventilation
Once the patient is apneic, you will mask ventilate. Some attendings will ask you to give a single breath to ensure that the patient can be ventilated, then intubate. Some will ask you to mask ventilate for a couple of minutes to ensure the lungs are truly filled with oxygen.
The patient’s airway can be made patent and the exchange of gases accomplished by holding an “air tight” mask over the patient’s nose and mouth while simultaneously performing a head tilt and jaw thrust maneuver. This is best done with the classic "C" and "E" hand position taught in BCLS (see below)

Using this technique the airway is not protected from possible aspiration. Ventilation can be entirely spontaneous by the patient, it can be assisted by the anesthesiologist, or it can be entirely controlled by the anesthesiologist. When giving positive pressure ventilation to a patient via face mask, it is important not to use excessive pressures (>20 cm H2O i.e. the opening pressure of the Lower Esophageal Sphincter) as this can cause distension of the stomach with air and increase the risk of gastric regurgitation. This is controlled by the turquoise knob next to the ambu-bag, which should be set to something below 20 while you bag.
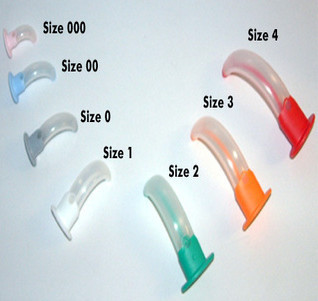
A common problem encountered with this technique is inadequate gas exchange due to obstruction of the airway by relaxed pharyngeal tissues. This obstruction can usually be overcome by the insertion of an oral-pharyngeal or nasopharyngeal airway.