1. What monitors should be available to ensure adequate patient oxygenation during anesthesia?
A pulse ox is used to tell if a patient is being adequately oxygenated. Alternatively, serial ABGs are also sometimes drawn to test for oxygenation. While pre-oxygenating a patient, the End Tidal CO2 is checked to ensure that >90% of the air being breathed out is oxygen (effectively washing out nitrogen from the lungs).
2. How is adequate patient ventilation monitored according to ASA standard?
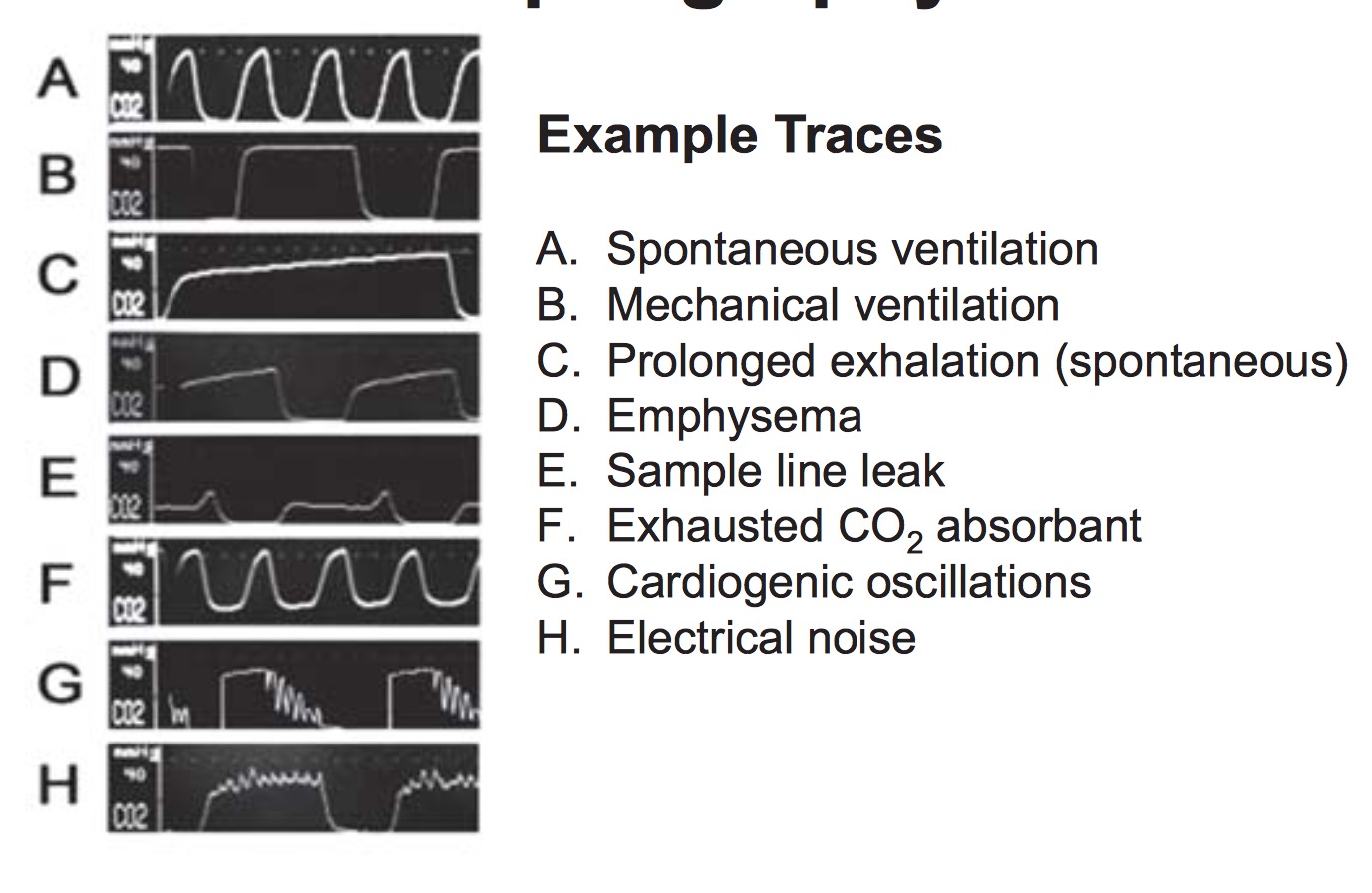
Ventilation (i.e. how much CO2 is given off) can be measured by capnography using a CO2 sampler. The sensor is usually connected to the airway circuit and samples the amount of CO2 the patient breathes out. It also forms a waveform.
3. In EKG monitoring why is the 5 lead system used in adults vs. the 3 lead system in children?
V5 detects ST changes secondary to ischemia. II is used to check rhythm (because p waves are highest in this lead). 5 Leads used in adults. 3 leads used in pediatric cases because ischemia is unlikely (so V5 is not essential).
4. What is the effect on the BP reading of placing a too small cuff on a patient?
- Too large = falsely LOW BP
- Too small = falsely HIGH BP.
5. When would you consider direct arterial pressure monitoring instead of a non-invasive method?
Indications for A-line:
- Accurate, beat to beat blood pressures are required. This includes situations where hypotension is a concern, or in morbidly obese patients.
- When non-invasive blood pressure measurement is not possible (e.g. burns or obesity).
- Serial ABGs are required.
- Serial blood sampling is required (e.g. in a patient undergoing a calcitonin-producing thyroid tumor removal).
6. What are the complications of arterial cannulation?
- Infection.
- Thrombosis.
- Hemorrhage.
- Embolism.
- Spasm
7. How does pulsoximetry work?
Pulse Oximetry measures the ratio of bright red oxygenated hemoglobin to darker red deoxygenated hemoglobin and displays this ratio as percent O2 saturation. Pulse oximeters do this by emitting two wavelengths of light, at 660nm and 940nm. The patterns of light absorption at these two wavelengths for the two types of hemoglobin are significantly different. Depending on how much light is absorbed or transmitted, the oximeter is able to determine saturation. The oximeter examines only the pulsatile component of the transmitted signal and therefore gives a level of arterial saturation.
8. Give examples of the factors which affect the accuracy of pulse oximetry.
Motion artifact, light artifact, pathologic hemoglobin (e.g. methemoglobin cannot be detected by pulse ox), certain dyes, medications, Hypotension (affects waveform).
9. What are the clinical uses of capnography?
Capnography measures the End Tidal CO2 expired by the patient. This can be used to detect:
- bronchospasm (upsloping trace)
- inadequate circulation resulting from hypotension indicating BP is too low for pt (number decreasing)
- pulmonary embolism (decreased number and increased difference between ETCO2 and PaCO2)
- adequacy of CPR eliminating need for pulse checks and compression interruption (ETCO2>10; if sudden increase in ETCO2, then likely have ROSC) -pt breathing * spontaneously (more rounded trace)
- esophageal intubation, circuit disconnect (no ETCO2 tracing)
- exhaused CO2 absorbent (ETCO2 does not return to 0-5)
10. Why do we monitor patient temperature? What is the mechanism for developing hyperthermia in an anesthesized patient?
Skin temperature regulates behavioral mechanisms (e.g. shelter, clothing, migration, etc). Core temperature determines autonomic responses (shivering, skin vasomotor activity, shivering). Under general anesthesia, autonomic responses compromise (as well as OR temperature and the vasodilation caused by anesthetics) lead to a decrease in core temperature. Hypothermia is associated with several poorer outcomes which may include worsened myocardial contractility, impaired coagulation, 3x increase in infection risk, delayed wound healing and delayed emergence.
11. Through what routes can temperature be measured in the OR?
Temperature can be measured through several methods (outlined below).
- Pulmonary Artery (gold standard)
- Bladder (not reliable if urine flow rate is low).
- Tympanic membrane (reflects brain temperature)
- Skin (variable accuracy depending on skin perfusion)
- Oropharynx (good estimate of core temperature; recent studies show correlation with tympanic and esophageal temperatures)
12. What are the advantages and uses for the BIS monitor?

The BIS uses EEGs to detect depth of anesthesia and consciousness, in theory to prevent awareness. It reports EEG activity on a 100 point scale. The meanings of BIS number are:
- 65-85 = sedation
- 30-65 = general anesthesia
- <30 = too deep
13. Discuss the causes, signs and management of different electrolyte abnormalities](ElectrolyteAbnormalities)
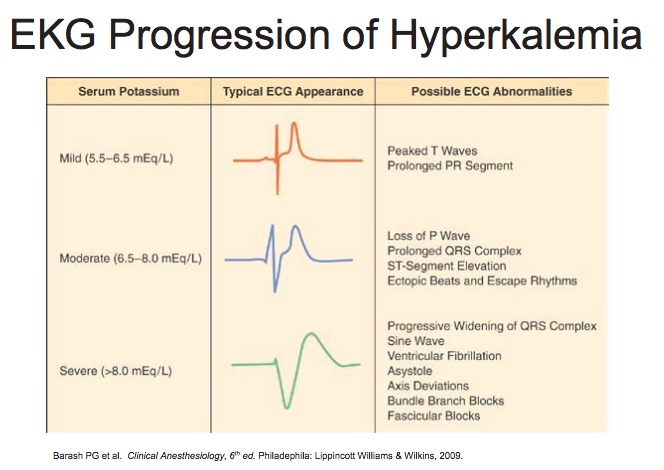
Hyperkalemia
-
Definition:
- Mild: 5.5-6.5
- Moderate: 6.5 - 8
- Severe: >8
-
Contributing Factors:
- Renal Disease
- Drugs (ACEi, NSAIDS, K-sparing diuretics, digoxin, B-Blockers)
- Succinylcholine (raises K by 0.5-1 acutely)
- Acidosis
- Hemolysis
- Rhabdomyolysis
- Administration of dantrolene and verapamil concurrently
- Hyponatremia, hypocalcemia
- Old pRBCs
-
Signs and Symptoms:
- Cardiac conduction system abnormalities, including cardiac arrest and dysrhythmias (usually requires K > 6). Classically associated with administration of succinylcholine to paralyzed or burn patients
- At K > 7, may have ascending paralysis that progresses to flacid paralysis and respiratory arrest
-
Treatment:
- Reverse membrane effects with Calcium
- Transfer extracellular K+ into cells with Bicarbonate (50-100 mEq over 5-10 min), Insulin (10-15 units) + Glucose (25g), and Beta 2 Agonists (albuterol)
- Remove potassium from body (Kayexelate, proximal or loop diuretics, dialysis).
-
Anesthetic considerations
- Consider canceling elective cases if K>5.5
- Avoid Succinylcholine
- Monitor for EKG changes
- Avoid hypoventilation (respiratory acidosis)
- Treat acidosis
- Consider NS instead of LR
- Monitor for increased sensitivity to muscle relaxants
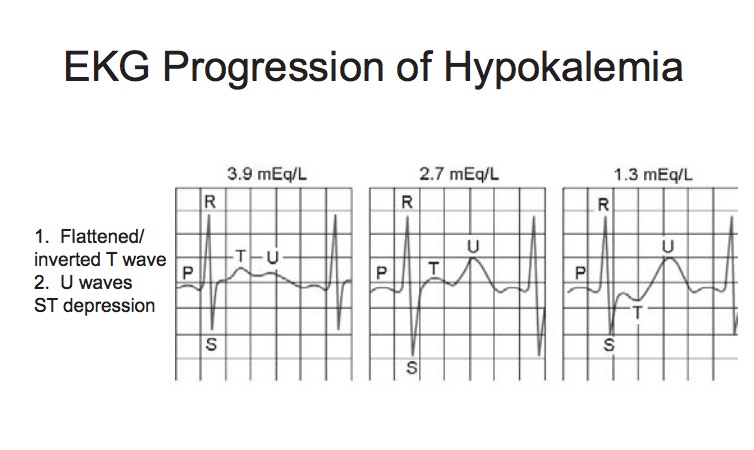
Hypokalemia
-
Definition:
- Mild: 3.1-3.5
- Moderate: K < 3 w/PACs
- Severe: K< 3 w/ PVCs
-
Preoperative Causes:
- GI Losses
- Lasix
- Magnesium Deficiency
-
Intraoperative Causes:
- Alkalosis
- Insulin
- Hypothermia
-
Signs and Symptoms:
- Acute Hypokalemia causes hyperpolarization of cardiac cells, leading to ventricular escape activity, re-entrant phenomena, ectopic tachycardias and delayed conduction.
- PACs, PVCs, SVTs (esp. A fib,/A flutter)
- Metabolic alkalosis
- Autonomic Lability
- Weakness, ↓ DTRs
- Ileus
- Digoxin toxicity
- Enhanced response to muscle relaxants
-
Treatment
- Chronic Hypokalemia:
1 mEq/L of K = 300-600 mEq total body deficit.
Acute Hypokalemia:
- Likely redistribution phenomenon
- Reverse underlying cause (e.g. alkalemia 2/2 mechanical hyperventilation)
-
Anesthetic Considerations:
- Consider cancelling elective cases if K<3-3.5 (depending on chronicity of defect).
- Monitor EKG for changes.
- KCL if arrhythmias develop
- Avoid hyperventilation (respiratory alkalosis)
- Consider reducing dose of muscle relaxant 25-50%
Hypercalcemia
-
Contributing Factors:
- Hyperparathyroidism
- Malignancy
- Immobilization
- Acute Renal Failure
- Drugs (Thiazide diuretics, lithium)
-
Signs and Symptoms
- EKG Changes (short QT)
- Hypertension
- Polyuria
-
Treatment
- Hydration
- Dialysis if severe/non-responsive
-
Anesthetic Considerations:
- Consider cancelling elective cases
- Avoid acidosis (reduces Ca2+/Albumin binding)
- Check serial K+ and Mg2+
Hypocalcemia
-
Preoperative Causes:
- Hypoparathyroidism
- Renal Failure (↓Vitamin D)
- Sepsis
- Magnesium Deficiency (Decreased end-organ response to PTH)
-
Intraoperative Causes:
- Alkalosis (increased Ca-Albumin binding)
- Massive pRBC binding (due to citrate binding)
- Drugs (heparin, protamine, glucagon)
-
Signs and Symptoms:
- EKG (prolonged QT, Bradycardia)
- Hemodynamics (vasodilation, hypotension, decreased myocardial contractility, LV failure)
- Respiratory (Laryngospasm, stridor, bronchospasm, respiratory arrest)
- Neuro (cramps, tetany, ↑DTR, perioral numbness, seizures)
-
Treatment:
- Calcium Gluconate - 1 g = 45 mEq elemental Ca2+ (do not give with bicarb; will precipitate)
- Replace Magnesium
-
Anesthetic Considerations
- Avoid alkalosis
- Monitor paralysis with muscle relaxants
Hypermagnesemia
-
Contributing Factors:
- Renal Failure
- Hypothyroid
-
Signs and Symptoms
- EKG (widened QRS, Prolonged PR interval, Bradycardia)
- Hemodynamics (vasodilation, hypotension, myocardial deprssion)
- Neuro (↓DTR, sedation, weakness, enhanced NM blockade)
-
Treatment
- Hydration
- Ca administration
-
Anesthetic Considerations
- Vigilance for EKG changes
- Consider reducing dose of muscle relaxants 25-50%
Hypomagnesemia
-
Contributing Factors
- GI/Renal losses
- Beta Agonists (cause intracellular shift)
- Drugs (diuretics, theophylline, aminoglycosides)
-
Signs and Symptoms
- Usually asymptomatic alone, but symptomatic in combination with induced hypokalemia, hypocalcemia, phyophosphatemia
- EKG (prolonged QT, PACs, PVCs, A Fib)
- Neuro (neuromuscular excitability, AMS, seizures)
-
Treatment
- Replace with MGSO4 to MG2+ > 2
- Watch for hypotension and arrhythmias with rapid administration.
-
Anesthetic Considerations
- EKG monitoring
- Check for coexistant electrolyte deficiencies.
14. Clinical Cases
68 y/o male with history of hypertension, diabetes, CAD with left bundle branch block and good functional capacity presents for intracranial aneurysm clipping.