Direct Laryngoscopy Procedure
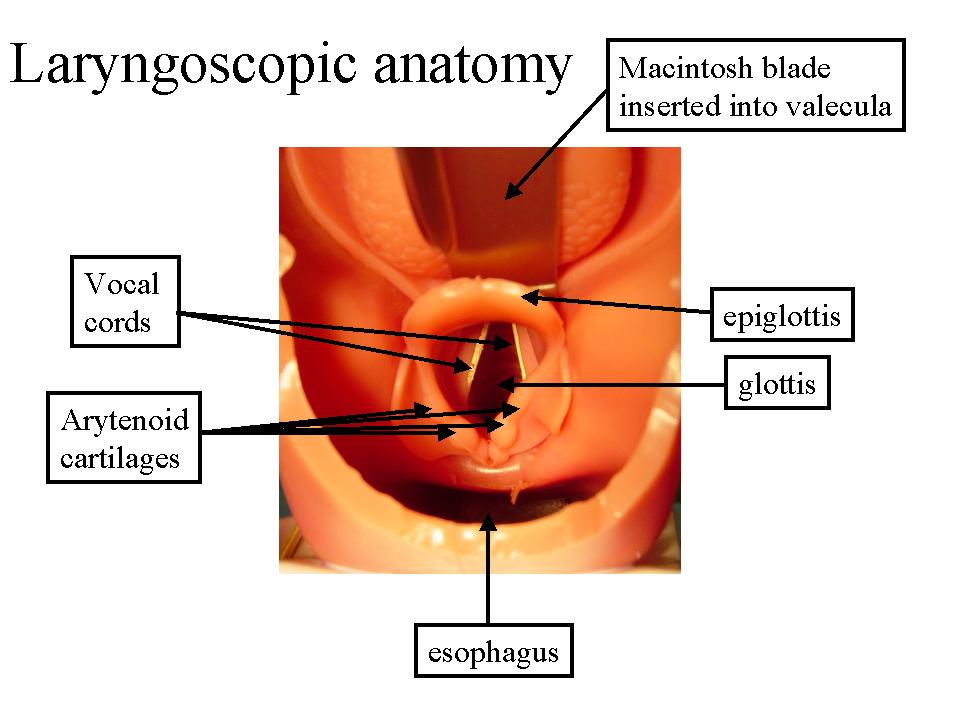
The procedure involves using a blade to visualize the larynx (laryngoscopy), then inserting a tube between the vocal cords. Here is the anatomy of the view you will obtain:
- Your attending and resident will teach you how to intubate correctly. However, here are a few helpful tips:
- Generally, adult women receive a 7.0 or 7.5mm internal diameter ETT and adult men receive a 7.5 or 8.0mm diameter ETT.
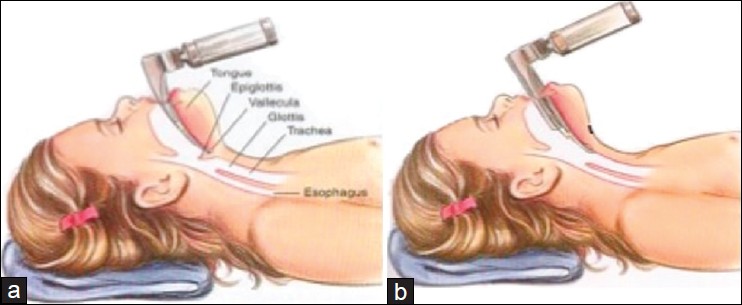
- Proper positioning will help immensely. Make sure the patient's head is extended towards you as much as possible (ask to remove some of the towels under their head if needed). The table should be up at least to the height of your navel.
- When scissoring open the mouth, do not be timid. Open the mouth as much as possible.
- The mac blade has a groove on the left that allowed you to sweep the tongue out of the way. Enter the patient's mouth diagnoally so that the tip of your blade is at the right border of the tongue, then straighten the blade to the center to sweep the tongue out of your view.
- Once you have inserted the blade in the mouth, your right hand is free. Use it to extend the patient's head to obtain a better view of the larynx.
- Applying Cricoid Pressure (which some attendings may call "External Laryngeal Manipulation") can help give you a better view. Ask for this if you can't get a good view.
- Often, the vocal cords will not actually be visible, so the artenyoid cartilages (see diagram above) will be the landmarks your should look out for.
- Once you obtain your view of the larynx, DO NOT LOOK AWAY. The attending and resident will hand everything to you.
- Tube is usually placed at the 20 - 24cm mark at the patient’s teeth. Deeper increases the risk of a right mainstem intubation.
Correct positioning of the endotracheal tube is confirmed by:
- Watching bilateral chest rise.
- Appearance of condensation in the endotracheal tube.
- Observing end tidal CO2 on the capnograph.
A detailed video of Direct Laryngoscopy can be found here.
Awake Intubation
Three classes of drugs are typically used to prepare the patient for an awake intubation, an antisialagogue is given to minimize airway secretions, mild sedation is given to minimize the patient’s response to stimulation, and local anesthetic is used directly on the airway. The airway can be anesthetized using a variety of approaches either alone or in combinations. Nebulized lidocaine can be inhaled by the patient for several minutes, the superior laryngeal nerves can be blocked transcutaneously, the mouth and posterior pharynx can be sprayed transorally with local anesthetic.
An excellent video of awake intubation is available here.
Complications
-
Traumatic Complications
- Airway Edema: Give dexamethasone after intubation to reduce swelling.
- Corneal Abrasion (by instruments): Cover eye with eye-tape.
- Bleeding: Suction blood to prevent aspiration.
-
Atraumatic Complications
- Laryngospasm (i.e. mechanical airway irritation -> closure of true vocal cords (protective mechanism against aspiration) - > hypoxia): Deepen anesthesia and try to break with positive pressure ventilation. If unsuccessful, give succinylcholine to relax the vocal cords. If that fails, prepare for a surgical airway.
- Esophageal Intubation: Remove the tube without insufflating and try again.
- Catecholamine release in response to intubation: Give fentanyl before intubation to blunt airway responses. Ensure anesthesia is at sufficient depth before intubating.
- Right Mainstem Bronchus: Make sure you see bilateral chest rise and hear bilateral breath sounds after intubating.