1. In relation to volatile anesthetics what does MAC mean? How is it useful?
Definition: Alveolar concentration of a gas at which 50% of subjects do not respond to surgical incision. The lower the MAC, the more potent the agent.
More Definitions:
MAC-awake: MAC necessary to blunt response to verbal stimulation (~0.4 MAC)
MAC-BAR: MAC needed to Blunt Autonomic Response to a noxious stimulus (~1.6 MAC).
MAC-EI: MAC needed to prevent laryngeal response to Endotracheal Intubation (~1.3 MAC).
2. Discuss the factors which increase and decrease MAC.
Increasing MAC:
- Drugs that increase central catecholamines.
- Acute cocaine and amphetamine use.
- Chronic EtOH abuse
- Hyperthermia (over 42C)
- Hypernatremia
- Redheaded females a 19% increased MAC.
- Younger age (greatest MAC requirement is in 10 year olds as hepatic metabolism is greatest in this age).
Decreasing MAC:
- Drugs that decrease central catecholamines.
- Chronic cocaine and amphetamine use.
- Acute EtOH abuse
- Hypothermia (50% decrease per 10C)
- Hypernatremia
- Pregnancy
- Hypotension (MAP <40 in adults)
- Hypoxemia (PaO2 < 38 mm Hg)
- Anemia
- Older age.
3. Does a lower blood-gas partition coefficient slow down or speed-up the rate of induction?
Blood:Gas Coefficient reflects the solubility of the gas in blood. The greater the coefficient, the greater the solubility, and the SLOWER the onset and offset of a gas.
This is because the anesthetic effect ONLY depends on the partial pressure of the gas, not the concentration in dissolved blood. The greater the percentage of gas that will become dissolved in blood (i.e. bound to plasma proteins), the longer it will take to reach the partial pressure necessary to induce anesthesia.
Similarly, the dissolved anesthetic gas in the blood acts as a reservoir that must be removed before the patient can wake up. Therefore, offset takes longer with the a larger coefficient.
4. How does cardiac output affect the rate of induction?
Inhaled anesthetics:
A high cardiac output leads to SLOWER inhalation induction. This is because gases in the alveoli do not have adequate time to equilibrate with the blood in the bloodstream.
IV Anesthetics:
A high cardiac output leads to FASTER IV induction. This is because IV induction agents reach the brain quicker.
Reverse is also true.
5. What is the second gas effect?
Nitrous Oxide is often given as an adjunct anesthetic with another volatile anesthetic for its dose-sparing effect. After both gases enter the Alveoli, Nitrous may rapidly diffuse into the blood stream, leaving behind a higher partial pressure of the second volatile anesthetic in the alveoli. This leads to a much stronger anesthetic effect than predicted with the second volatile anesthetic alone.
6. What is diffusion hypoxia?
A decrease in PAO2 when the patient is emerging from an inhalational anesthetic where N2O was a component. Rapid outpouring of N2O into the alveoli can displace alveolar oxygen, resulting in hypoxia.
7. Why is N2O use avoided in the presence of a closed pneumothorax?
N2O can diffuse into closed cavities (e.g. penumothorax, bowel, middle ear, etc) faster than Nitrogen can diffuse out. This can expand the cavity or increase the pressure in a closed space.
8. Discuss the effects of inhaled anesthetics on mean arterial pressure, cardiac output, and SVR.
Mean Arterial Pressure: All agents cause a dose related decrease in Blood Pressure by ↓ SVR. Halothane and Sevoflurane decrease cardiac output, but other agents have no effect on it.
Arrhythmias: Halothane increases incidence of arrhythmias.
9. What are the effects of inhaled anesthetics on ventilation? What happens to the ventilatory response to CO2 and O2?
Ventilation: All agents ↑ Respiratory Rate and ↓ Tidal Volume. In addition, the ventilation response to Hypercarbia and Hypoxia becomes blunted.
10. What are the effects of inhaled anesthetics on cerebral blood flow and CMRO2?
Cerebral Blood Flow: All agents ↑ cerebral blood flow (via direct vasodilation) and ↓ Cerebral Oxygen Demand (CMRO2).
11. How do inhaled Anesthetics affect ICP?
All agents ↑ ICP.
12. What is malignant hyperthermia, how does it present, how is it managed?](MalignantHyperthermia)
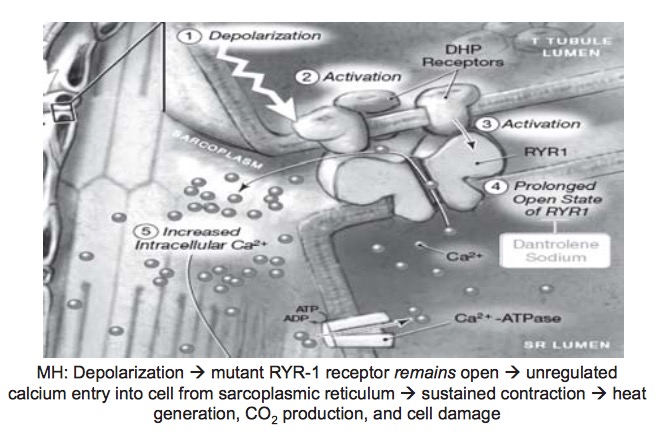
Definition: A hypermetabolic crisis that occurs when susceptible patients are exposed to a triggering anesthetic agent; underlying defect is abnormally increased Ca2+ levels in skeletal muscle causing acceleration of muscle metabolism.
Mechanism
Presentation
(In sequence of occurance).
- Muscle rigidity (first masseter i.e. 'trismus', then total body rigidity) - due to increase cytoplasmic free Ca2+.
- Increased CO2 production (most sensitive + specific sign). Increased O2 consumption and heat production - due to hypermetabolism.
- Hyperkalemia - due to cell damage.
- Tachycardia, hypertension, cutaneous vasoconstriction, - due to increased catecholamines.
- ↑ Cardiac Output - due to metabolic acidosis and decreased PaO2.
- ↑ Ventilation - Increased ETCO2.
- (Late and inconsistent sign of MH). Temperature rise (1C every 5 min).
- Arrythmias, DIC, Hemorrhage, Cerebral Edema, Renal Failure, Compartment Syndrome, Death (due to DIC and organ failure).
Differential
- Neuroleptic Malignant Syndrome (NMS) (in patients receiving antidopaminergic agents or in withdrawal from dopamine agents as in Parkinson’s)
- Thyroid Storm (would not see hyperkalemia or acidosis)
- Sepsis (b/c see fever, tachypnea, tachycardia, metabolic acidosis)
- Pheochromocytoma (↑HR,↑BP, but normal EtCO2 and Temp)
- Drug-induced (e.g. ecstasy, crack, amphetamines, PCP, LSD)
- Serotonin Syndrome (associated drugs interactions MAOIs + merperidine or MAOIs+ SSRIs)
- Iatrogenic Hyperthermia
- Hypercarbia from CO2 insufflation for laparoscopy.
Treatment
-
Immediate:
- D/C Volatile agents and Sux.
- 100% O2
- Halt surgery ASAP.
- Place Foley (as dantrolene formulation contains mannitol).
- Give Dantrolene! Keep giving until signs of MH are controlled - Titrate to HR/CO2. Dantrolene works by interfering with excitation-contraction coupling by binding to the RYR-1 Ca2+ channel.
-
Treat Acidosis
- Hyperventilate patient.
- Bicarbonate.
-
Treat Hyperthermia
- Cool if T >39 C
- Apply cold NS via IV.
-
Treat Hyperkalemia
- Calcium (to stabilize cardiac membranes).
- Hyperventilate (ventilate out CO2).
- Insulin + Glucose (to increase cellular potassium uptake).
- Bicarbonate.
-
Treat Dysrhytmias
- Standard therapies but avoid CCBs in presence of Dantrolene as may promote hyperkalemia.
-
Maintain Urine Output
- Lasix to establish diuresis and prevent ARF.
-
Monitor:
- ETCO2
- Temperature
- UOP + Color (myoglobinuria can turn urine dark)
- Eletrolytes
- ABG
- CK
- PT/PTT/INR