1. Give reasons for establishing central venous access.
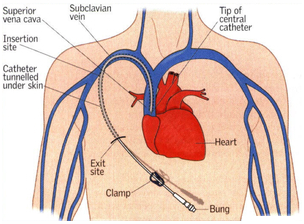
- Sits in subclavian or internal jugular with tip directed towards SVC.
- Measures RAP RVEDP = RV preload and thought to parallel LAP and thus LV preload.
- Inaccurate in patients with pulmonary HTN, Right heart disease, valvular pathologies, pulmonary edema, PEEP (↑ intrathoracic pressure during expiration ↑ CVP)
- Also used to infuse inotropes or vasopressors
2. Describe some causes of preoperative hypovolemia.
- NPO Status
- Vomiting
- Diarrhea
- Bowel Prep
- Fever
- Sepsis
- Trauma
- Fluid shifts (e.g. burns, ascites, pleural effusion)
3. How is intravascular fluid volume evaluated?
Not very reliable:
- HR and BP (control for PPV and anesthetics may cause relative hypovolemia)
- Pulse Oximetry (waveform wanders from baseline)
- Urine Output (stress response from surgery increases ADH so not reliable measure).
- Serial ABGs to check lactate.
Reliable in the absence of heart pathology
- Central Venous Catheter (for CVP).
Very reliable:
- Pulmonary artery catheter: Most commonly used for in RV dysfunction, pulmonary hypertension, valvular pathology (AS, MR), LV dysfunction.
- Transesophageal Echocardiogram: Commonly used in major cardiac surgeries and liver transplants.
4. Calculate the maintenance fluid requirements for a 70 kg man.
Maintenance: Generally 4-2-1 rule is used. 4ml/hr/kg for first 10 kg, 2 ml/hr/kg for next 10 kg, 1 ml/hr/kg for each additional kg.
For a 70 kg man, the total fluid requirements are 4 x 10 kg + 2 x 10 kg + 1 x 50 kg = 110 ml/hr.
5. This man has been NPO for 8 hrs. How do these affect intraoperative fluid maintenance requirements?
Compensation for pre-existing fluid deficits: Multiply maintenance requirements by the number of hours NPO. Give 1/2 of additional fluids in the first hour, 1/4 in the 2nd hour, and 1/4 in the 3rd hour.
If the man in the example above has been NPO for 8 hours, he needs an additional 880 ml (for a total of 990 ml). 440 ml (on top of the maintenance 110 ml) will be given in the first hour of the surgery. 220 ml (+110 ml maintenance) will be given in each of the next two hours).
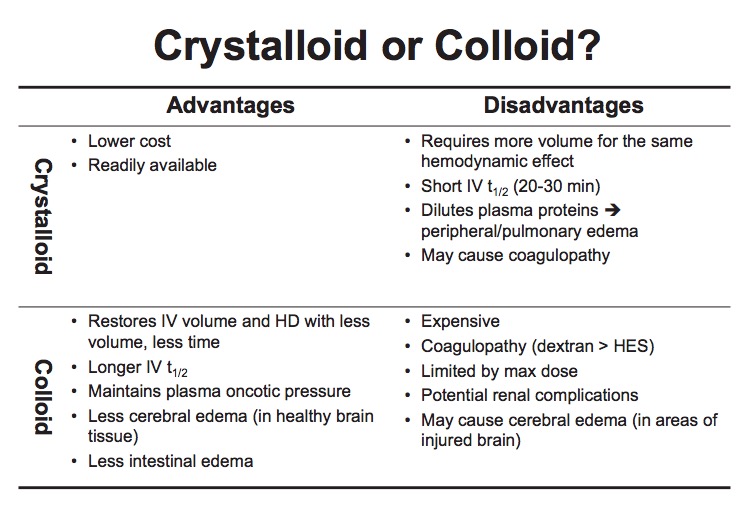
6. What complications are associated with the use of colloids?
7. What are the ASA guidelines for blood transfusion?
Hg < 6 in young, healthy patients. (Patient and practitioner variability)
-
At Hgb 6-10 g/dl, the decision to transfuse is based on:
- Ongoing signs of organ ischemia
- Potential or ongoing blood loss
- Volume status
- Risk factors for vulnerability to low O2.
8. What fluid is given with blood transfusions?
Normal Saline is used because:
- LR: Theoretical clot formation due to calcium.
D5W: hypotonic solutions (less than 0.9% saline → hemolysis).
What are the guidelines for FFP transfusion?
Urgent reversal of Coumadin
- Correction of known factor deficiency
- Correction of 1) microvascular bleeding with INR > 1.5, 2) INR > 2, or 3) PTT > 2x normal
- During massive transfusion (before lab results available)
- Heparin resistance (i.e. antithrombin III deficiency) in patients requiring heparinization