Hyperkalemia
-
Definition:
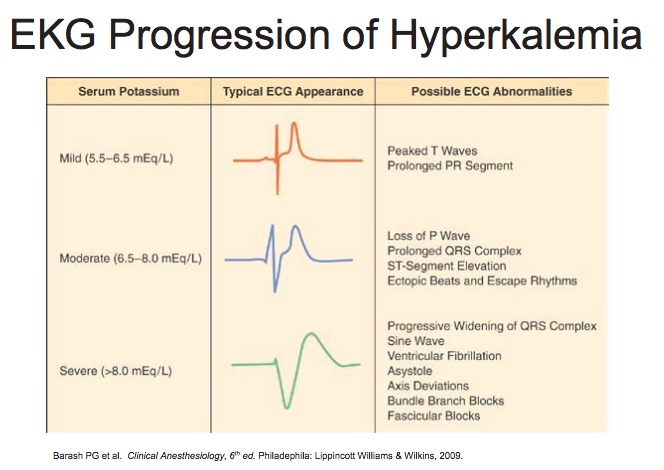
- Mild: 5.5-6.5
- Moderate: 6.5 - 8
- Severe: >8
-
Contributing Factors:
- Renal Disease
- Drugs (ACEi, NSAIDS, K-sparing diuretics, digoxin, B-Blockers)
- Succinylcholine (raises K by 0.5-1 acutely)
- Acidosis
- Hemolysis
- Rhabdomyolysis
- Administration of dantrolene and verapamil concurrently
- Hyponatremia, hypocalcemia
- Old pRBCs
-
Signs and Symptoms:
- Cardiac conduction system abnormalities, including cardiac arrest and dysrhythmias (usually requires K > 6). Classically associated with administration of succinylcholine to paralyzed or burn patients
- At K > 7, may have ascending paralysis that progresses to flacid paralysis and respiratory arrest
-
Treatment:
- Reverse membrane effects with Calcium
- Transfer extracellular K+ into cells with Bicarbonate (50-100 mEq over 5-10 min), Insulin (10-15 units) + Glucose (25g), and Beta 2 Agonists (albuterol)
- Remove potassium from body (Kayexelate, proximal or loop diuretics, dialysis).
-
Anesthetic considerations
- Consider canceling elective cases if K>5.5
- Avoid Succinylcholine
- Monitor for EKG changes
- Avoid hypoventilation (respiratory acidosis)
- Treat acidosis
- Consider NS instead of LR
- Monitor for increased sensitivity to muscle relaxants
Hypokalemia
-
Definition:
- Mild: 3.1-3.5
- Moderate: K < 3 w/PACs
- Severe: K< 3 w/ PVCs
-
Preoperative Causes:
- GI Losses
- Lasix
- Magnesium Deficiency
-
Intraoperative Causes:
- Alkalosis
- Insulin
- Hypothermia
-
Signs and Symptoms:
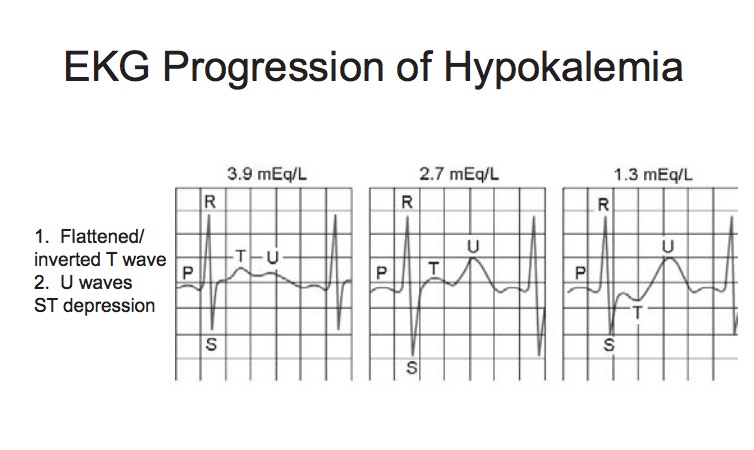
- Acute Hypokalemia causes hyperpolarization of cardiac cells, leading to ventricular escape activity, re-entrant phenomena, ectopic tachycardias and delayed conduction.
- PACs, PVCs, SVTs (esp. A fib,/A flutter)
- Metabolic alkalosis
- Autonomic Lability
- Weakness, ↓ DTRs
- Ileus
- Digoxin toxicity
- Enhanced response to muscle relaxants
-
Treatment
- Chronic Hypokalemia:
1 mEq/L of K = 300-600 mEq total body deficit.
Acute Hypokalemia:
- Likely redistribution phenomenon
- Reverse underlying cause (e.g. alkalemia 2/2 mechanical hyperventilation)
-
Anesthetic Considerations:
- Consider cancelling elective cases if K<3-3.5 (depending on chronicity of defect).
- Monitor EKG for changes.
- KCL if arrhythmias develop
- Avoid hyperventilation (respiratory alkalosis)
- Consider reducing dose of muscle relaxant 25-50%
Hypercalcemia
-
Contributing Factors:
- Hyperparathyroidism
- Malignancy
- Immobilization
- Acute Renal Failure
- Drugs (Thiazide diuretics, lithium)
-
Signs and Symptoms
- EKG Changes (short QT)
- Hypertension
- Polyuria
-
Treatment
- Hydration
- Dialysis if severe/non-responsive
-
Anesthetic Considerations:
- Consider cancelling elective cases
- Avoid acidosis (reduces Ca2+/Albumin binding)
- Check serial K+ and Mg2+
Hypocalcemia
-
Preoperative Causes:
- Hypoparathyroidism
- Renal Failure (↓Vitamin D)
- Sepsis
- Magnesium Deficiency (Decreased end-organ response to PTH)
-
Intraoperative Causes:
- Alkalosis (increased Ca-Albumin binding)
- Massive pRBC binding (due to citrate binding)
- Drugs (heparin, protamine, glucagon)
-
Signs and Symptoms:
- EKG (prolonged QT, Bradycardia)
- Hemodynamics (vasodilation, hypotension, decreased myocardial contractility, LV failure)
- Respiratory (Laryngospasm, stridor, bronchospasm, respiratory arrest)
- Neuro (cramps, tetany, ↑DTR, perioral numbness, seizures)
-
Treatment:
- Calcium Gluconate - 1 g = 45 mEq elemental Ca2+ (do not give with bicarb; will precipitate)
- Replace Magnesium
-
Anesthetic Considerations
- Avoid alkalosis
- Monitor paralysis with muscle relaxants
Hypermagnesemia
-
Contributing Factors:
- Renal Failure
- Hypothyroid
-
Signs and Symptoms
- EKG (widened QRS, Prolonged PR interval, Bradycardia)
- Hemodynamics (vasodilation, hypotension, myocardial deprssion)
- Neuro (↓DTR, sedation, weakness, enhanced NM blockade)
-
Treatment
- Hydration
- Ca administration
-
Anesthetic Considerations
- Vigilance for EKG changes
- Consider reducing dose of muscle relaxants 25-50%
Hypomagnesemia
-
Contributing Factors
- GI/Renal losses
- Beta Agonists (cause intracellular shift)
- Drugs (diuretics, theophylline, aminoglycosides)
-
Signs and Symptoms
- Usually asymptomatic alone, but symptomatic in combination with induced hypokalemia, hypocalcemia, phyophosphatemia
- EKG (prolonged QT, PACs, PVCs, A Fib)
- Neuro (neuromuscular excitability, AMS, seizures)
-
Treatment
- Replace with MGSO4 to MG2+ > 2
- Watch for hypotension and arrhythmias with rapid administration.
-
Anesthetic Considerations
- EKG monitoring
- Check for coexistant electrolyte deficiencies.