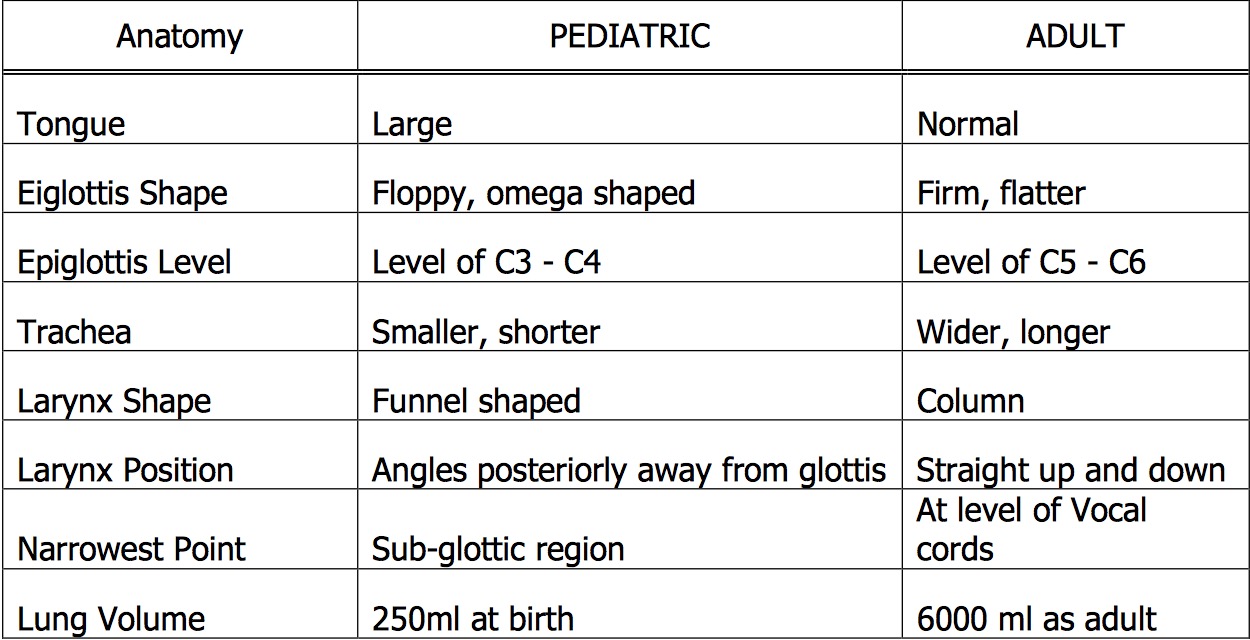
The respiratory mechanism of the pediatric patient varies from the adult in both anatomy and physiology. As children grow, the airway enlarges and moves more caudally as the c-spine elongates. The pediatric airway overall has poorly developed cartilaginous integrity allowing for more laxity throughout the airway. Another important distinction is the narrowest point in the airway in adults is at the cords versus below the cords for children. Some of the important anatomic differences are listed below.

An important aspect of the narrow airway in children is that resistance is significantly increased. The formula to consider is
R ~ 8l / r4
R – resistance, l – length, r – radius
Small changes in the airway radius will therefore increase the resistance to the fourth power. Therefore, a small amount of post-extubation sub-glottic edema will significantly increase the work of breathing for an infant. Children also have a smaller forced residual capacity (FRC) defined as the residual volume plus the expiratory reserve volume. Physiologically, FRC occurs when the outward pull of the chest wall equals the inward collapse of the lungs.
FRC essentially acts as a respiratory reserve. When patients begin to develop respiratory distress, an increased FRC equates to a longer period of time prior to respiratory failure. The reduced FRC is important in two particular circumstances. First, it can be decreased by up to 30% in a supine patient as compared to a sitting patient. As the abdominal contents push up on the diaphragm in a supine patient, the FRC is affected. This situation is amplified in pediatric patients because of a compliant chest wall, small thoracic cage, and large abdominal contents. Second, while pre-oxygenating a patient prior to intubation the reduced FRC decreases the amount of time allowed to establish an endotracheal tube prior to desaturation.
There are also many physiologic differences in respiratory mechanisms between children and adults. Children have a more complaint trachea, larynx, and bronchi due to poor cartilaginous integrity. This in turn allows for dynamic airway compression, i.e. a greater negative inspiratory force “sucks in” the floppy airway and decreases airway diameter. This in turn increases the work of breathing by increasing the negative inspiratory pressure generated. A vicious cycle is created which may eventually lead to respiratory failure: subglottic stenosis ⇒ ⇑ negative inspiratory force ⇒ airway collapse ⇒ ⇑ subglottic stenosis ⇒ ⇑ negative inspiratory force ⇒ ⇑ work of breathing ⇒⇒ respiratory failure. Pediatric patients also have more compliant chest walls also increasing the work of breathing – i.e. the outward pull of the chest is greater.
Infants are dependent on functional diaphragms for adequate ventilation. The accessory muscles contribute less to the overall work of breathing in infants as compared to older children and adults. Therefore, a non-functional diaphragm often leads to respiratory failure. Diaphragmatic fatigue is one amongst several potential causes of respiratory failure and apnea in young patients with RSV bronchilitis.
Finally, the respiratory muscles themselves have a significant oxygen and metabolite requirement in children. In pediatric patients the work of breathing can account for up to 40% of the cardiac output, particularly in stressed conditions.
This cursory discussion of the pediatric respiratory anatomy and physiology allows one to appreciate the significant differences between children and adults. Therefore, the child with respiratory distress / failure should be approached and treated with urgency, vigilance, and caution.